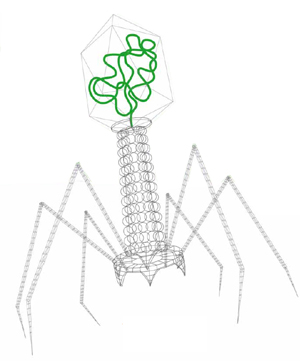
Bacteriophages
Bacteriophages are some of the most abundant life forms on earth, and are programmed exclusively to infect and identify host bacteria. Phages have co-evolved with bacteria for more than a billion years and are able to survive in the most extreme environments including soil, animal waste and intestinal tracts. Research shows that phages offer a number of advantages over antibodies, such as superior specificity and superior binding, when used in microbiological test systems. Phage proteins have been proven to provide robust performance in many different applications, even when challenged with the most demanding and complex food matrices.
Campylobacter
The number of enteric infections caused by Campylobacter genus - and Campylobacter jejuni (thermo tolerant bacterium) in particular - has been rising rapidly ever since many countries set up monitoring systems. The complications related to these infections - bacteraemia, secondary infections and Guillain-Barré syndrome (neurological complication) - are now well documented and can be particularly severe. Campylobacter is the third cause of death from food borne infections after Salmonella and Listeria. Campylobacter is found primarily in warm-blooded animals, particularly poultry. Transmission to humans usually occurs through eating insufficiently cooked contaminated foods (poultry, mutton, pork) and exposure to contaminated water and environments in food production facilities and animal breeding facilities (primarily poultry farms).The frequent presence and high level of Campylobacter in such samples, the lack of regulations in most countries and the complex analyses required are all factors that have, until now, hampered routine screening.
Clostridium difficile
The incidence and severity of Clostridium difficile have increased significantly over the past 10 years, since a strain of this bacterium originating in North America acquired a new virulence. C. difficile now causes about 250,000 hospitalizations and at least 14,000 deaths every year in the United States. With the ability to produce greater quantities of toxins A and B, this new strain is more resistant to the antibiotic group known as fluoroquinolones, and has now also spread to European countries.
To find out more consult our dedicated website BE S.M.A.R.T WITH RESISTANCE
Enterobacteriaceae
Increasing emphasis on a total quality approach in food production, HACCP plans and Risk Assessment procedures enhance the role that quality indicators such as Total Viable Count, Coliforms, Escherichia coli and Enterobacteriaceae have in monitoring the hygienic and commercial quality of food.
Enterobacteriaceae enumeration is the key hygiene parameter in the latest European regulation on microbiological criteria for food, EC 2073/2005. The Enterobacteriaceae family includes important food spoilage agents and certain intestinal pathogens such as Salmonella spp., Shigella spp…
Escherichia coli O157
The severity of Escherichia. coli O157:H7-induced infection, generally caused by the consumption of contaminated meat or milk, is now well-established. Standard food hygiene and storage precautions are frequently not enough to limit the presence of this micro organism. Screening for this pathogen is now more important than ever.
Enterobacter sakazakii (Cronobacter)
A neonatal pathogen associated with the powdered infant formula (PIF). The organism has been isolated from various food products as well as from environmental sources, such as water and soil (Fanning & Forsythe, 2007). It has been found in foods, including milk powder, chocolate, cereal, spices and pasta. Enterobacter sakazakii is also an occasional contaminant of dehydrated foods. In neonates it can cause a rare, but life threatening form of neonatal meningitis (10-55% fatality), bacteraemia, necrotizing enterocolitis (NEC) (40-80% fatality) and necrotizing meningo-encephalitis (Bowen & Braden, 2006). Enterobacter sakazakii is a member of the Enterobacteriaceae family and was designated as a new bacterial species by Farmer et al., in 1980. Recently, the taxonomy of E. sakazakii was clarified and a reclassification of E. sakazakii was proposed which groups 6 species into a new genus, Cronobacter (submitted for publication in IJSEM*). * International Journal of Systematic and Evolutionary Microbiology
Legionella
Legionella is a pathogenic bacterium that is the causative agent of Legionnaire’s disease also known as legionellosis. The disease is a serious form of pneumonia and can be fatal if not diagnosed and treated early. Infection is acquired by inhaling Legionella-contaminated aerosols from sources such as cooling towers, spas and showers. The at risk populations are essentially male adults with associated risk factors such as immunodeficiency, smoking, alcoholism or diabetes. In 2005, over 1,500 legionellosis cases were reported in France and approximately 5,700 in Europe. According to the CDC (Centers for Disease Control and Prevention), an estimated 8,000 to 18,000 cases of legionellosis occur each year in the United States.
Listeria
Members of the genus Listeria are ubiquitous and only one species is pathogenic. Listeria have been isolated from various food products including dairy products, meat, vegetables, and seafood, as well as from environmental samples taken, in particular, from food processing plants. Listeria monocytogenes is the only species considered as pathogenic for humans. Listeriosis in humans may cause pathologies such as meningitis, septicaemia, encephalitis and abortions. Groups at risk include pregnant women, neonates, immunocompromised patients, and the elderly. Listeria monocytogenes is widespread in the environment and is a potential risk when raw, partially processed and even some fermented food are consumed.
Methicillin-resistant Staphylococcus aureus (MRSA)
Mycobacterium avium ssp paratuberculosis
Mycobacterium avium ssp paratuberculosis (MAP) is the etiological agent of Johne’s disease, a granulomatous enteritis that can affect cattle, sheep and goats and other non-ruminant wildlife species. Numerous countries have set up programs to control this major digestive disease but with different levels of success. Heterogeneity of fecal samples, low shedders and PCR inhibitions are the main issues for a trustable direct detection of paratuberculosis infected animals.
Solution for Paratuberculosis detection